Disclaimer: This website and application are intended for research and informational purposes only.
We do not assume any responsibility for how the content, services, or tools provided on this site are used.
Any unauthorized or improper use of this application is the sole responsibility of the user.
We disclaim any liability for damages, losses, or issues arising from misuse or unintended use.
Heparin prediction form
Recommandations
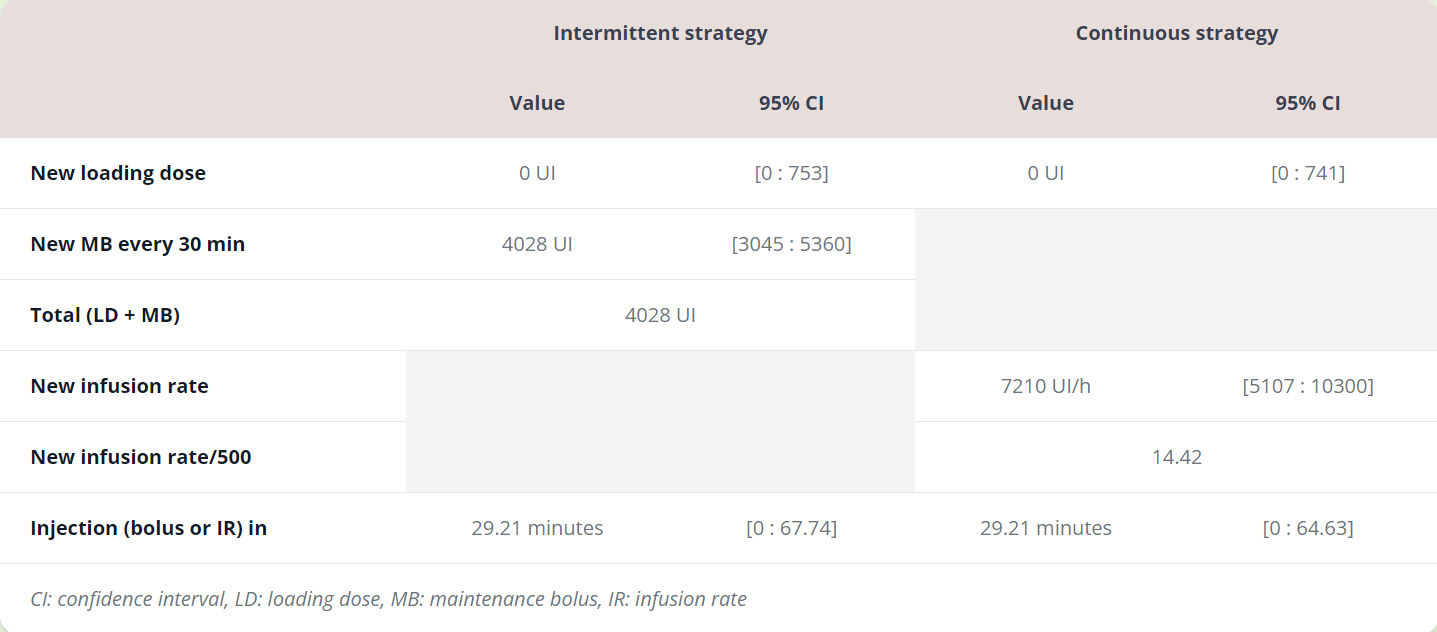
| Intermittent strategy | Continuous strategy | |||
|---|---|---|---|---|
| Value | 95% CI | Value | 95% CI | |
New loading doseThe loading dose corresponds to the ammount of UFH to administer in a bolus to reach the target ACT value.For example, if the last ACT measurement is above the target ACT, no loading dose should be required. If the last measured ACT is below the target ACT, a UFH bolus dose recommandation will be provided to reach the target. For an intermettint bolus strategy: a maintenance bolus should be added to the loading dose to stay above the target ACT during your specified period of time. For a continuous strategy: a UFH infusion should be given to stay at the target ACT level. |
||||
New maintenance bolusThe maintenance bolus corresponds to the ammount of UFH to administer for the ACT to be above the target ACT for the desired time (the time between bolus injections in minutes in the form). |
||||
Total (LD + MB)This ammount corresponds to the total UFH bolus to administer in one bolus in order to:1) reach the target ACT (thanks to the loading dose) and 2) if you are using the intermittent strategy, to stay above the target ACT (thanks to the maintenance dose) for the period of time you have defined in the form (time between bolus injections in minutes). |
||||
New infusion rateAfter the target ACT is reached, the new infusion rate corresponds to the continuous UFH infusion rate in IU per hour to administer to stay at the target ACT during the surgery. |
||||
New infusion rate/500This is simply the new infusion rate divided by 500 |
||||
Injection (bolus or IR) inThis corresponds to the time to wait in minutes before the next UFH doses to admnister.For example, if the last measured ACT is below the target ACT, the time will indicate 0, meaning that you can now administer the next dose of UFH. If the last measured ACT is above the target ACT, you will have to wait some time before needing to administer the next dose. |
||||
Protamine, end of surgeryCorresponds to the amount of protamine to administer at the end of the surgery. |
||||
| CI: confidence interval, LD: loading dose, MB: maintenance bolus, IR: infusion rate | ||||
| Intermittent strategy | ||
|---|---|---|
| Value | 95% CI | |
New LDThe loading dose corresponds to the ammount of UFH to administer in a bolus to reach the target ACT value.For example, if the last ACT measurement is above the target ACT, no loading dose should be required. If the last measured ACT is below the target ACT, a UFH bolus dose recommandation will be provided to reach the target. For an intermettint bolus strategy: a maintenance bolus should be added to the loading dose to stay above the target ACT during your specified period of time. For a continuous strategy: a UFH infusion should be given to stay at the target ACT level. |
||
New MBThe maintenance bolus corresponds to the ammount of UFH to administer for the ACT to be above the target ACT for the desired time (the time between bolus injections in minutes in the form). |
||
Total (LD + MB)This ammount corresponds to the total UFH bolus to administer in one bolus in order to:1) reach the target ACT (thanks to the loading dose) and 2) if you are using the intermittent strategy, to stay above the target ACT (thanks to the maintenance dose) for the period of time you have defined in the form (time between bolus injections in minutes). |
||
Injection inThis corresponds to the time to wait in minutes before the next UFH doses to admnister.For example, if the last measured ACT is below the target ACT, the time will indicate 0, meaning that you can now administer the next dose of UFH. If the last measured ACT is above the target ACT, you will have to wait some time before needing to administer the next dose. |
||
ProtamineCorresponds the amount of protamine to administer at the end of the surgery. |
||
| Continuous strategy | ||||
|---|---|---|---|---|
| Value | 95% CI | |||
New LDThe loading dose corresponds to the ammount of UFH to administer in a bolus to reach the target ACT value.For example, if the last ACT measurement is above the target ACT, no loading dose should be required. If the last measured ACT is below the target ACT, a UFH bolus dose recommandation will be provided to reach the target. For an intermettint bolus strategy: a maintenance bolus should be added to the loading dose to stay above the target ACT during your specified period of time. For a continuous strategy: a UFH infusion should be given to stay at the target ACT level. |
||||
New IRAfter the target ACT is reached, the new infusion rate corresponds to the continuous UFH infusion rate in IU per hour to administer to stay at the target ACT during the surgery. |
||||
New IR/500This is simply the new infusion rate divided by 500 |
||||
Injection inThis corresponds to the time to wait in minutes before the next UFH doses to admnister.For example, if the last measured ACT is below the target ACT, the time will indicate 0, meaning that you can now administer the next dose of UFH. If the last measured ACT is above the target ACT, you will have to wait some time before needing to administer the next dose. |
||||
ProtamineCorresponds the amount of protamine to administer at the end of the surgery. |
||||
| CI: confidence interval, LD: loading dose, MB: maintenance bolus, IR: infusion rate | ||||
Tutorial
1 - Setup
Patient weight
|
Target ACT (s)
400
Time between bolus injections (min)
30
Section 1:
Enter the patient's body weight in kg.
Enter the target ACT recquired by the surgery, the ACT threshold you wish to be at or above, in seconds.
Enter the time between heparin bolus injections in minutes for the intermittent bolus dosing regimen, such as every 30 or 60 min.
Those informations are mandatory for the models to compute.
2 - ACT
ACT measurement
120
Time
30/10/2024 10:10
ACT measurement
380
Time
30/10/2024 11:00
ACT measurement
|
Time
30/10/2024 11:20
Section 2:
Enter the ACT measurements in seconds, with their measurement times (date, hour and minutes), in chronological order.
Those informations are mandatory for the models to compute.
3 - Heparin bolus injections
Heparin bolus
10000
Time
30/10/2024 10:50
Heparin bolus
|
Time
30/10/2024 11:15
Sections 3 and 4:
Enter the time of administration and amount of administered UFH bolus in UI.
Enter the start time, duration in minutes and infusion rate in UI per hour of UFH infusions administered.
Run calculations:
Press to calculate an optimized UFH dosing regimen based on ACT measurements.
The results contain dosing recommendations for both Intermittent UFH dosing strategy (based on iterative bolus) and continuous UFH dosing strategy (based on continuous infusion).
Please note that only data from your last session is saved, and only locally. You can recover you last session by pressing Load last session.
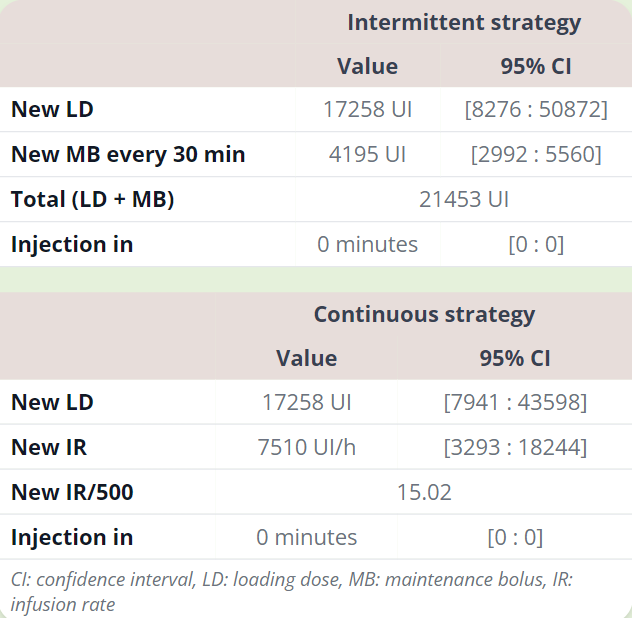
Table interpretation:
The table presents the model's recommandations for both an intermittent UFH dosing strategy and a continous UFH dosing strategy.
The loading dose (LD) corresponds to the intravenous UFH bolus to administer to reach the desired target ACT if the last measured ACT was below the ACT target.
The maintenance bolus (MD) corresponds to the intravenous UFH bolus to administer to stay above the desired ACT target threshold during the period of time defined in section 1 (example: MB to administer every 30 or 60 minutes to stay above target ACT).
Total (LD + MD) is the sum of the loading dose and the maintenance bolus to admninister for the intermittent dosing strategy.
For the continuous dosing strategy, the infusion rate (IR) corresponds to the UFH infusion rate in UI per hour to keep the ACT values at the desired ACT target during surgey.
Finally, for both dosing strategies, the last table row corresponds to the time to wait before the next recommended LD, MD and IR to administer. This waiting time starts at the time of the last measured ACT.
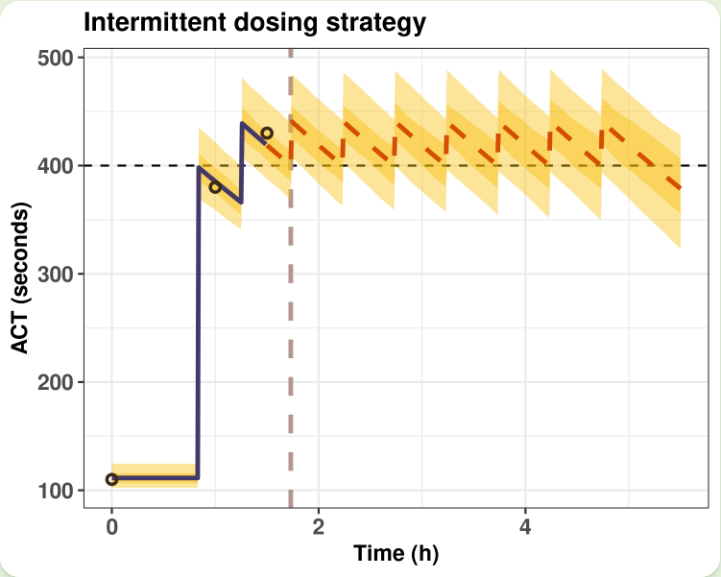
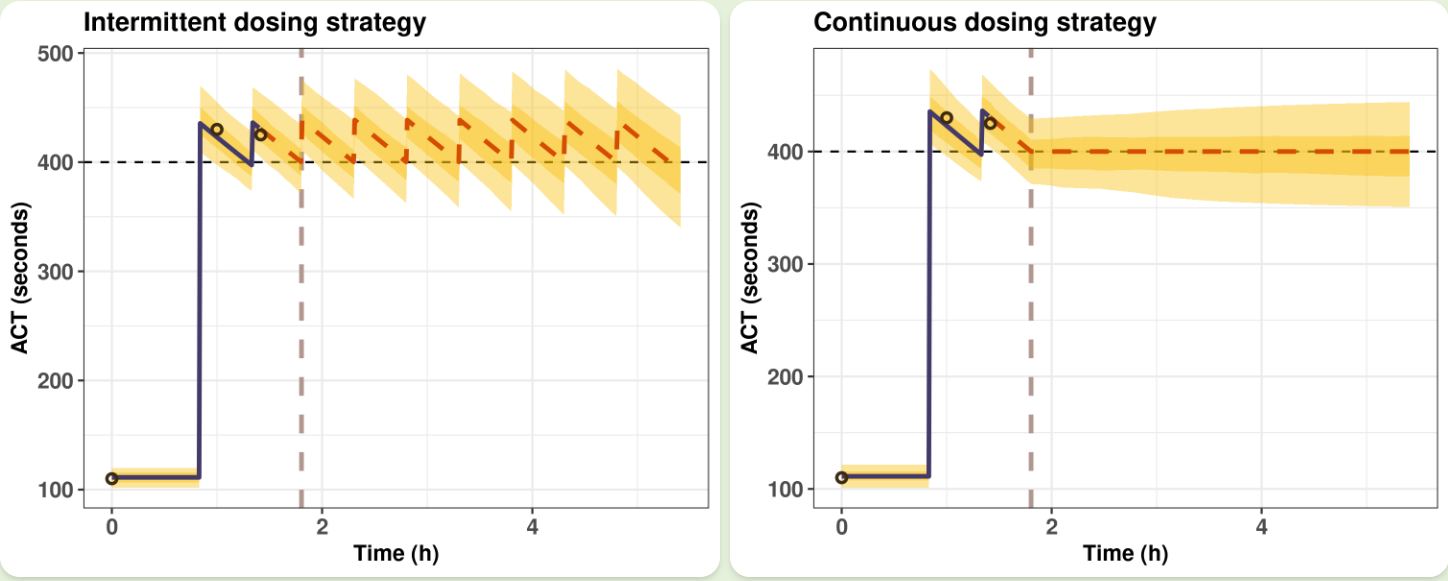
Plot interpretation:
The horizontal black dotted line represents the target ACT threshold chosen for the surgery.
The brown circles represent the measured ACT values.
The blue solid line corresponds to fitted ACT values using dosing history, patient body weigth and ACT measurements.
The red dotted line corresponds to predicted ACT values using the individualized UFH dosing regimen, continuous or intermittent.
The vertical brown dotted line represents the time for the next injection, LD, MB and or IR.
The golden yellow ribbons correpond to the 50% and 90% confidence intervals.
Methodology:
The pharmacodynamic models of UFH during cardiac surgery used in this application were developed using pharmacodynamic data from more than 200 patients. The models were developed using non-linear mixed effect modelling approach, and are robust to outlier ACT measurements.
All details concerning the pharmacokinetic models are presented in the bibliography section.
With the scientific support of:



Bibliography
Chaux R, Lanoiselée J, Magand C, Zufferey P, Delavenne X, Ollier E. Robust K-PD model for activated clotting time prediction and UFH dose individualisation during cardiopulmonary bypass. Comput Methods Programs Biomed. feb 2022;214:106553
Abstract
Background and objective: Activated clotting time (ACT) is a point-of-care test used to monitor the effect of unfractionated heparin (UFH) during cardiopulmonary bypass (CPB). This test sometimes returns aberrant values, which can lead to the administration of an inappropriate dosing regimen. The development of a population-robust K-PD model of UFH could allow the individualisation and automation of UFH therapy during CPB.
Methods: We conducted a prospective observational study to collect ACT measurements from patients undergoing surgery using CPB. The ACT data were split into a development and validation cohort. The development cohort was used to estimate a standard and robust population K-PD model characterised by a residual error following a normal distribution and student's t-distribution. The ACT prediction performance using Bayesian estimates of individual K-PD parameters was evaluated by comparing predicted versus observed ACTs. Using estimates of the robust K-PD model, a Bayesian individualisation strategy to automate UFH administration was proposed and evaluated using Monte Carlo simulations.
Results: A total of 295 patients were included in the study, and 1561 ACTs were collected. In patients without outlier values, Bayesian estimates (based on four ACT measurements) from both standard and robust K-PD models had similar performances, with a median prediction bias close to 0 s. In patients with outlier measurements, the use of the robust K-PD model greatly improved the prediction bias and root-mean-square error (RMSE), with a mean prediction bias of 3.25 s, IQR = [-19.9; 46.03] versus -86 s IQR = [-135.7; -63.8] for the standard model. Monte Carlo simulations showed that the robust Bayesian individualisation strategy allowed the ACT to be maintained above the target using only two to three ACT measurements.
Conclusions: The use of a robust K-PD model reduced prediction bias and RMSE in patients with outlier ACT measurements. The Bayesian individualisation strategy using robust estimates of individual parameters may help automate UFH dosing regimens. Proper clinical validation is warranted before its use in daily clinical practice.
Gibert A, Lanoiselée J, Gouin-Thibault I, Pontis A, Azarnoush K, Petrosyan A, et al. Factors Influencing Unfractionated Heparin Pharmacokinetics and Pharmacodynamics During a Cardiopulmonary Bypass. Clin Pharmacokinet. jan 2 2024
Abstract
Background and objective: Unfractionated heparin (UFH) is commonly used during cardiac surgery with a cardiopulmonary bypass to prevent blood clotting. However, empirical administration of UFH leads to variable responses. Pharmacokinetic and pharmacodynamic modeling can be used to optimize UFH dosing and perform real-time individualization. In previous studies, many factors that could influence UFH pharmacokinetics/pharmacodynamics had not been taken into account such as hemodilution or the type of UFH. Few covariates were identified probably owing to a lack of statistical power. This study aims to address these limitations through a meta-analysis of individual data from two studies.
Methods: An individual patient data meta-analysis was conducted using data from two single-center prospective observational studies, where different UFH types were used for anticoagulation. A pharmacodynamic/pharmacodynamic model of UFH was developed using a non-linear mixed-effects approach. Time-varying covariates such as hemodilution and fluid infusions during a cardiopulmonary bypass were considered.
Results: Activities of UFH's anti-activated factor/anti-thrombin were best described by a two-compartment model. Unfractionated heparin clearance was influenced by body weight and the specific UFH type. Volume of distribution was influenced by body weight and pre-operative fibrinogen levels. Pharmacodynamic data followed a log-linear model, accounting for the effect of hemodilution and the pre-operative fibrinogen level. Equations were derived from the model to personalize UFH dosing based on the targeted activated clotting time level and patient covariates.
Conclusions: The population model effectively characterized UFH's pharmacokinetics/pharmacodynamics in cardiopulmonary bypass patients. This meta-analysis incorporated new covariates related to UFH's pharmacokinetics/pharmacodynamics, enabling personalized dosing regimens. The proposed model holds potential for individualization using a Bayesian estimation.